Abstract
Background and Aim: Acute graft versus host disease (aGVHD) remains a major problem after allogeneic hematopoietic stem cell transplantation (allo-SCT). Steroids currently represent the gold-standard treatment for aGVHD based on prospective randomized trials, while fewer than half of patients have a lasting complete response. The long-term mortality rate of steroid-refractory (SR) aGVHD remains around 70%. To date, no consensus has been reached regarding the optimal salvage treatment for SR-aGVHD. We performed the first prospective, multi-center clinical trial to assess the efficacy and safety of the combination of ruxolitinib and etanercept as a novel approach to treat grades II-IV SR-aGVHD .
Methods: Thirty-one malignant hematologic disease patients with grades II-IV SR-aGVHD after allo-SCT from three centers in East China were enrolled from January 2017 to January 2018. All of them received ruxolitinib and etanercept as salvage-therapy for SR-aGVHD. Ruxolitinib was initiated at a dose of 5-10 mg BID for 2 months, and then tapered gradually for another one month. Etanercept was administrated at 25mg BIW for 2-8 weeks.
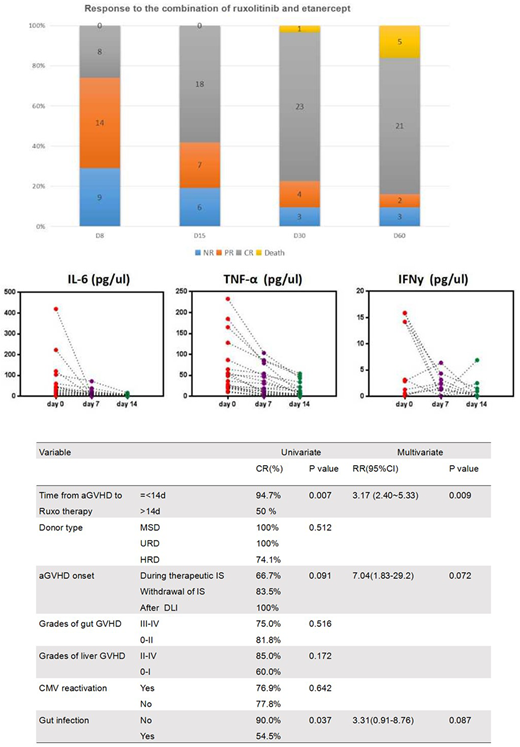
Results: At day 30 after starting the combination treatment, overall response (complete and partial response: CR+PR) was 90.3% with 74.2% being CR. The incidences of CR per organ were 93.5%, 84.2% and 82.6% for skin, liver, and gut involvement, respectively. The median time from combination therapy to the optimal response was 12 days.
The patients who received ruxolitinib within 14 days after aGVHD onset have a higher CR rate that those with delayed ruxolitinib therapy (94.7% vs. 50.0%, p=0.007). And the patients without gut infections have a higher CR rate than infected cohort (90.0% vs. 54.5%,p=0.037). Only time from aGVHD to ruxolitinib (RR=3.17, 95%CI 2.40~5.33, p=0.009) were independent predictors for incomplete response. III-IV Cytopenia and CMV-reactivation were observed during ruxolitinib treatment in 29.0% and 41.9% of patients. A significant decline in the level of IL-6, IFN-y and TNF-α was observed during 2-week treatment. The number of peripheral effector Tregs and Treg/Th17 ratio were significantly increased in responding patients.
Compared with the historical cohort of basiliximab and etanercept for SR-aGVHD in our center (n=31), no significant difference was found on the baseline, such as age, gender, underlying disease, disease status, conditioning intensity, as well as SR-aGVHD characteristics. Although the ORR in patients treated with ruxolitinib and etanercept is identical with the historical cohort (90.3% vs. 90.3%), ruxolitinib group achieved rapider remissions in liver aGVHD and gut aGVHD than the historical cohort (median time to remission for liver aGVHD: 21days vs. 28 days, p=0.0049; median time to remission for gut aGVHD: 11 days vs. 17 days, p=0.0026).
Among 31 patients in the study cohort, 9 cases (29.0%) were complicated with severe infection >= 2 grade, including military tuberculosis(n=1), CMV-interstitial pneumonia(n=1), carbapenem-resistant enterobacteriaceae (CRE) sepsis(n=2), invasive fungal infection (IFI,n=1), human herpesvirus-6 acute limbic encephalitis (n=1) and bacteria pneumonia (n=3). The 1-year overall survival (OS) and 1-year non-relapse mortality (NRM) were 73.9% and 22.9%, respectively, and the 1-year relapse rate was 8.3% after ruxolitinib.
Conclusion: Combined treatment with ruxolitinib and etanercept resulted in a rapid CR to visceral aGVHD and meanwhile reserve graft anti-leukemia (GVL) effect as the relapse rate of primary disease is relatively lower. The various infection complications associated with ruxolitinib merit more attention.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal